Stooped Posture: Signs, Causes, and Treatment
Several routines and automatic activities of the body
are affected due to Parkinson’s. This includes simple activities like standing
straight.
What
is it stooped posture?
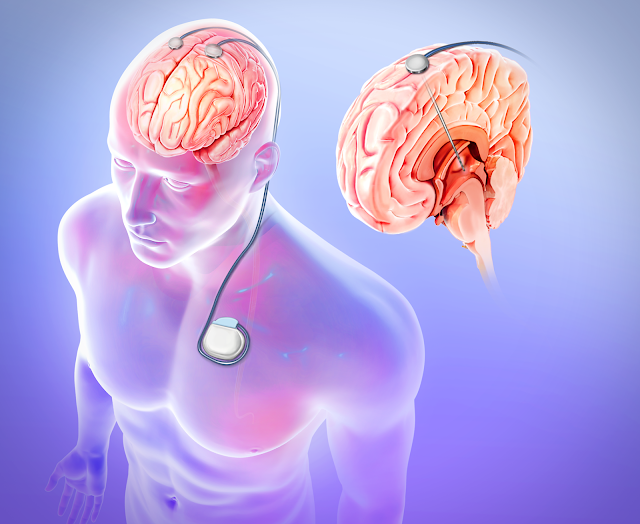
Normally, our brain controls all our body movements
and sends regular reminders to various body parts. However, due to Parkinson’s
disease, the brain loses the ability to send automatic reminders.
As a result, the body parts show involuntary
movements.
This includes a change in posture also, as the brain
is not able to send automatic reminders to stand straight. These changes in
posture may have various symptoms like stooped posture, rounded shoulders,
decreased low back curve, or forward lean of the head or trunk, which makes a
patient look hunched over.
Causes of stooped posture:
For a patient suffering from Parkinson’s, a change of posture may occur, due to any of the following reasons:
- Stiffness of muscle or rigidity
- The ‘off’ phase, where your medication is not working properly
- After being in a particular position for too long, which happens when the patient is involved in some work like reading or watching TV
- If the patient is concentrating on another activity, such as walking or working at the computer
Effects of stooped posture:
Though stooped posture is not a medical problem in itself, still it is important for a patient suffering from Parkinson’s to try and maintain an upright posture. This is because; a stooped posture can lead to other negative effects and medical problems. Some of these challenges are listed below:
- When the spine curves are out of alignment, a patient may experience severe pain in the neck or the back.
- Stooped posture reduces the ability of the patient to take deep breaths. This adversely affects the ability of the patient to speak clearly and loudly.
- Due to the stooped posture, a patient with Parkinson’s is not able to make eye contact while talking with anyone. The problem gets compounded due to facial masking and lowered voice. This can have a big negative impact on the self-confidence of the patient and the patient’s ability to communicate with others.
- The loss of flexibility in the body and difficulty in changing posture can make it very difficult for the patient to do simple routine work. The patient faces problems while raising arms overhead while wearing a shirt or getting up out of a chair.
- A poor posture can disturb the body balance of the patient, and may lead to falling down.
Treating Stooped Posture:
There is no medication to treat stooped posture. However, a patient may use the following tricks in order to maintain a good posture:
- Keep checking the posture (both front and side view), by standing in front of the mirror. This exercise should be done several times throughout the day.
- Be aware of any change in your posture. Try to catch yourself while the body is stooping or leaning. Take corrective actions to control it. Take help from people around you, by asking them to point out to you, in case they notice you stooping.
- Be aware of the problem of stooping. Hence, keep changing your position regularly. Take frequent breaks while working, and have a change in your movement.
- While sitting, use supports like back (lumbar) or neck (cervical) rolls or cushions for better postural alignment.
- Stooped posture reduces the flexibility of the muscles in the front part of the body less flexible and also weakens the muscles in the back of the body. Hence, it is advised to perform simple posture exercises and body stretches several times during the day, whenever you get time.
- The patient may consider joining a yoga class or even a Tai Chi class. Tai Chi, commonly known as ‘Shadowboxing’ is an internal Chinese martial art, which is used for defense training, health benefits, and meditation.
- consult a doctor or a therapist for getting physical therapy done, which involves doing specific exercises and recommending postures to help you manage stooped posture.
Conclusion:
Parkinson’s disease creates a disorder in the nervous system of the body. As a result, the brain loses its control over various body movements. One of these is body posture. The patient tends to lean forward, have a stoop, or rounded shoulders, which makes a patient look hunched over. While there are no medicines, there are some lifestyle-related techniques, exercise, and therapies that can help manage stooped posture.
For more information visit - https://parkinsons.co.in/